Sponsoring Institutional Framework
The WRIGHT place to learn and grow
The Wright Center for Graduate Medical Education created a living sponsoring institution education framework that details why and how we do what we do as a Teaching Health Center and what makes Teaching Health Centers special places to learn and grow the physician workforce America needs.
A rapidly evolving healthcare landscape necessitates the deployment of an anticipatory graduate medical educational model that aligns with patient and community needs, accreditation, and regulatory compliance to ensure the entry of safe, competent practitioners who are well-prepared to meet the increasingly complex care of patients and the communities in which they serve
Pioneering and unique learning opportunities include dental services, behavioral health, addiction & recovery services – including Medication Assisted Treatment – a Ryan White HIV and Infectious Disease Clinic, an Alzheimer’s and Dementia Unit, a Mobile Outreach Unit, a holistic Lifestyle Medicine program and an emerging Street Medicine program.

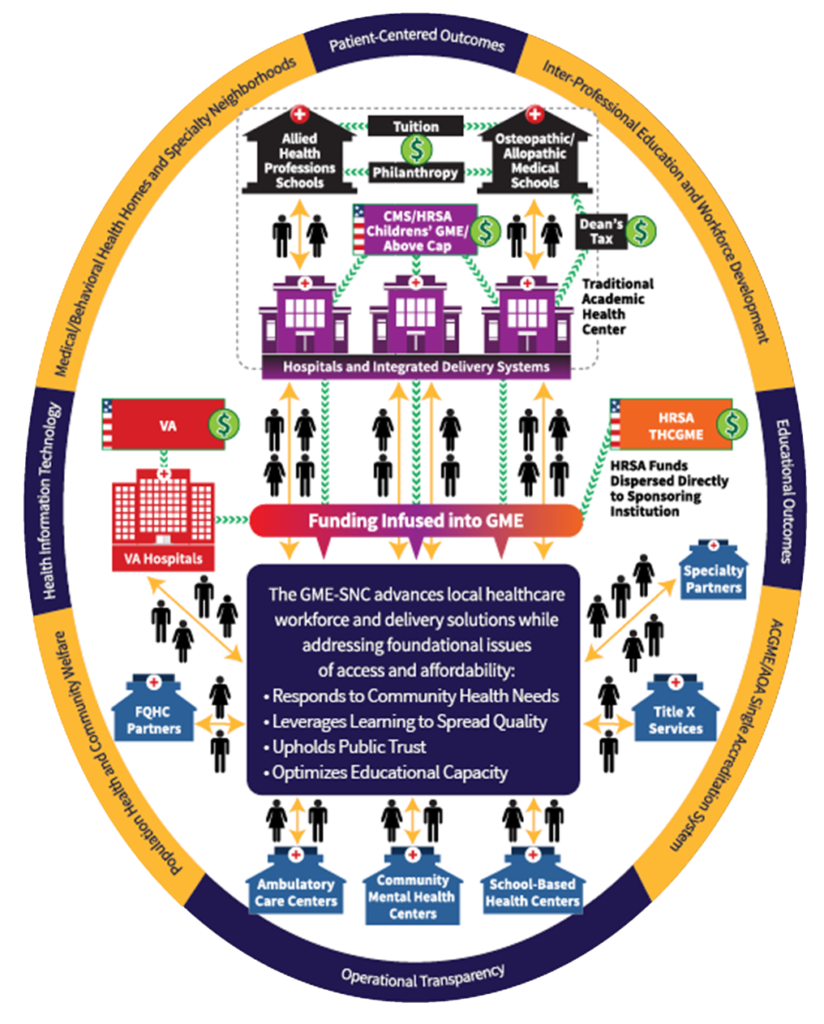
Our GME-SNC Model
Our Graduate Medical Education Safety-Net Consortium (GME-SNC) was built on great faith that community-governed consortium models can actualize the vision of Community Health Academic Medical Partnerships (CHAMPs).
Funded by all three federal GME agencies, we deliver strategic, inter-professional workforce development through enriched community partnerships, aligned for excellent, accountable care to promote the health and welfare of individuals, families and communities.