The Wright Center for Community Health Scranton Practice is hosting an American Red Cross blood drive on Friday, Feb. 9, to honor a city police detective injured in a January shooting.
Regional residents can make an appointment to donate blood between 11 a.m. and 4 p.m. at The Wright Center’s Scranton Practice, 501 S. Washington Ave., by visiting redcross.org and using sponsor code: The Wright Center or call 1-800-RED-CROSS.
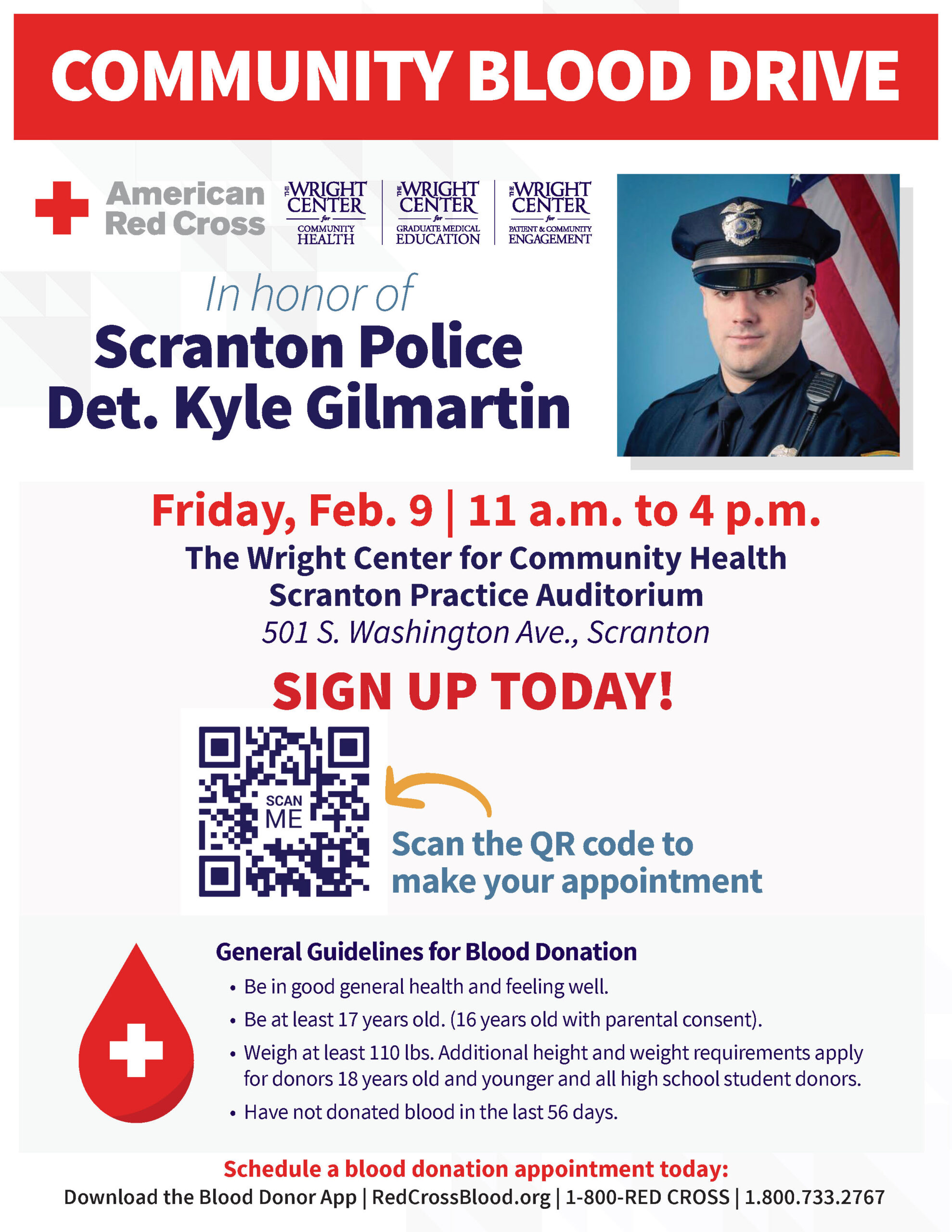
The drive is in honor of Scranton police Detective Kyle Gilmartin, who was shot on Jan. 11 in West Scranton. He and other Scranton police officers were investigating a pair of gang-related gunfire incidents at the time. After being treated at Geisinger Community Medical Center, Detective Gilmartin is recovering at a rehabilitation center.
“As a medical organization, we want to help where the need is greatest, and January is a time when there are critical blood shortages here and nationwide,” said Gerri McAndrew, co-director of The Wright Center for Patient & Community Engagement. “We know that treating Detective Gilmartin required a lot of blood, so we thought hosting a blood drive in his honor would be fitting.”
In addition to helping address the blood shortage, anyone who donates blood in February will receive a $20 Amazon gift card by mail.
Headquartered in Scranton, The Wright Center operates 10 primary and preventive care practices, including a mobile medical and dental vehicle called Driving Better Health, in Northeast Pennsylvania. Its practices offer integrated whole-person care, meaning patients typically have the convenience of going to a single location to access medical, dental, and behavioral health care, as well as community-based addiction treatment and recovery services.