Whole-Person Wellness: Need a check-in?


Need a check-in?
At the beginning of April we talked about Community Meeting, the Sanctuary meeting opening procedure during which we ask one another in turn how are you feeling, what is your goal, and who can you ask for help? If someone answers that first question in a way that they are feeling less than good, we follow up by asking if they need a check-in conversation.
Consider this our check-in.
I should be doing other things at this moment, as there are a lot of deadlines for a lot of folks for a lot of things. However, The Wright Center committed to the Sanctuary journey and it has been a minute since we’ve shared a moment.

I don’t know about you, but it has been an absolutely bat guano few weeks. (Guano is another word for, uhm, well, excrement.) Things have been so out of pocket, in fact, that I actually took a moment last week to see if there was some sort of cosmic activity that would explain the absolutely unhinged nature of what has been going on. Because it wasn’t just me, and it wasn’t just at work. It seemed to be everywhere. Reenactment triangles building Epcot Centers everywhere all at once.
In truth, human beings are doing this to one another all over the place all the time. To paraphrase the late novelist Toni Morrison, it happens so easily and so often, it isn’t really even all that interesting. To react, to spin out, to feel badly and transfer that to others, to avoid, to blame – all very common. I’m personally guilty of these things, for sure. It is very human to do this stuff. We all get tired, hungry, irritable, and frustrated. Some of us have health issues that are exacerbated by things that don’t seem to bother other people as much. Layer this with trauma triggers, and before you know it you have those Epcots springing up all over.
Any good psychologist will tell you it gets worse before it gets better, and perhaps we have a little of that going on as well. Awareness is a necessary first step, and the challenge of awareness is actually becoming aware of the problem space(s). If we are dissociated, avoidant, unengaged, it is easy to ignore, to pretend the thing isn’t real or doesn’t exist. Much like the selective attention test, once you see what you didn’t before, you can’t really believe you missed it. And you’ll never miss it again.
Awareness can be a trap, particularly if it accompanies our triggers. Sometimes we can find ourselves aware only of our trauma responses and mistake those for the emotional flashes from which our trauma is trying to protect us.
Anger, avoidance, helplessness, fawning – all of these feel very legitimate, because they are. They are very effective mechanisms for people who have no other options. What we hope to do in trauma work is help ourselves, our colleagues, our patients, and our communities to see that adults have choices. We may not like them. They may be difficult and hard to swallow, like parboiled brussel sprouts. But they do exist, and some of them are really healthy.
There is a lot going on. A lot of change, a lot of intense work. The Core Team is gearing up, and soon more steady beats of Sanctuary tools and milestones will be coming, as will a whole slew of new residents, new patients, new weather, new opportunities, and maybe even some new choices.

QUICK TIP
The work of de-escalation happens everywhere – even, and perhaps especially, in the clinic. This quick tip is thanks to Dr. Stephanie Gill, who shared the following Patient-Oriented Evidence that Matters (POEM) article. Its wisdom can be applied to anyone who is feeling dysregulated, including ourselves.
Steps to recognize and manage angry and disruptive patients
Clinical Question
How should clinicians manage angry and disruptive patients?
Bottom Line
To recognize and manage the angry patient, the authors of this commentary encourage prior planning and a calm demeanor. The commentary has several recommendations on what to do and what not to do.
The original article is not research but provides action steps we can use in our offices. Patients often present signs of increased anxiety prior to verbal and physical aggression. Being able to recognize these signs may help identify situations that can be de-escalated prior to further aggression. Given how common interactions with angry patients are in health care, it is recommended to not only come up with an action plan on how to respond to these situations, but also to rehearse these scenarios ahead of time. The following de-escalation techniques are useful components of this type of plan.
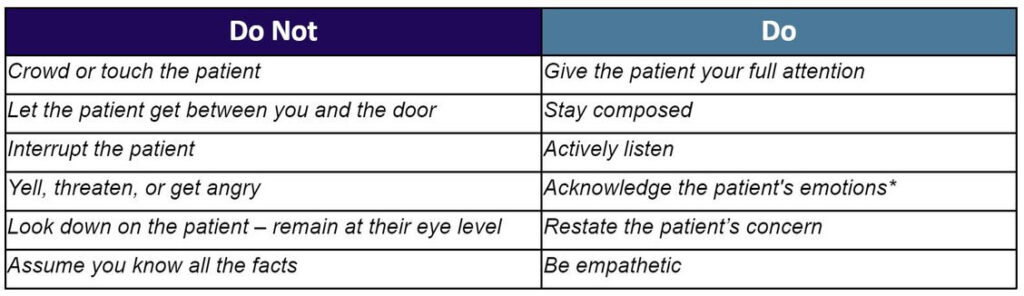
*If the patient is yelling or threatening, inform the patient that you are leaving the room and will return when they are calmer.
Finally, the authors recommend debriefing with the office staff after an incident and modifying the plan, if necessary. Although this approach does not appear to have been studied, it seems like a reasonable framework.
References:
Sincerely,
Meaghan P. Ruddy, Ph.D.
Senior Vice President
Academic Affairs, Enterprise Assessment and Advancement,
and Chief Research and Development Officer