Suicide prevention

Suicide: Why aren’t we talking about it more?
Suicide is one of the leading causes of death worldwide, so why aren’t we discussing it more? Stigma can have a dramatic impact on starting the conversation. We might feel reluctant or even ashamed to speak about our thoughts and feelings, which perpetuates the cycle.
When I was only 20 years old, I was grieving a loss and deeply struggling with substance use and financial problems. I remember feeling hopeless and worthless. I tried taking my own life.
I had grown up with the fear of talking about what I was feeling or experiencing, even with the support of loved ones. Now, I have come to understand there is great strength in talking about your feelings. It allows others to feel less alone, it takes the pain and anguish out of your physical body, and it connects you to others. We all will experience depression, loss, anxiety, or stress at some point in our lives. Remember, you are important, you are heard, and you are never alone.
Please take a moment to review these statements and decide whether you believe each to be a myth or a fact:
- Asking a person about suicide will encourage the person to attempt suicide.
- Once a person is considering suicide, there is nothing you can do.
- A person who attempts suicide will always be suicidal.
- Suicide happens without warning.
Each statement provided above by the National Council for Mental Wellbeing is a MYTH.
Why each statement is a myth:
- When asking about suicide, we should always be direct. This can allow the individual to open up and feel comfortable about their feelings, as well as decrease the stigma surrounding suicide.
- Most people who are at risk feel suicidal for only a brief period of their lives.
- Most crises are associated with significant levels of distress and are time-limited.
- There are typically many warning signs regarding suicide and suicidal ideation.
Risk Factors and Warning Signs
Risk factors can include:
- Previous suicide attempt(s)
- A history of suicide in the family
- Substance use
- Mood disorders (depression, bipolar disorder, etc.)
- Losses and other events (for example, the breakup of a relationship or a death)
- History of trauma or abuse, including historical trauma
- Bullying
- Chronic physical illness, including chronic pain
- Social isolation
- Stigma associated with seeking help
Some warning signs can include:
- Talking or writing about death, dying, or suicide.
- Hopelessness, decreased sense of purpose in life, saying things like, “It would be better if I wasn’t here.”
- Increased alcohol and/or drug use
- Withdrawal from loved ones and community
- Reckless/impulsive behavior
- Dramatic mood shifts
- Talking about being a burden to others or feeling trapped
- Giving away possessions
(Source: American Psychiatric Association)
Language regarding suicide:
Take a moment to think about why we would say a person “died by suicide” instead of “committed” or “successful” suicide.
When we use the word “committed,” we are implying this is a crime or something sinful. When we use the word “successful,” we are insinuating suicide to be something positive. The language in our society has many underlying negative connotations and once again perpetuates the stigma surrounding suicide.
Let’s change how we view and act towards suicide and bring awareness to the person who is deeply suffering.
Self-harm or Nonsuicidal Self-Injury
- Self-harm is when someone intentionally hurts themselves.
- This can be through cutting, burning, scratching, hitting oneself, and other forms.
- Not everyone who self-harms has the intent to kill themselves, however, they can be at higher risk.
- Those who self-harm can experience intense emotions and find a sense of relief through hurting themselves.
- Physical injury can trigger endorphin release
- Some who self-harm say it is a way to feel when experiencing emotional numbness
Symptoms and warning signs:
- Scars
- Fresh bruises, cuts, or burns
- Frequent reports of accidental injury
- Wearing long sleeves or pants, especially in warm weather
- Emotional and behavioral instability and impulsivity
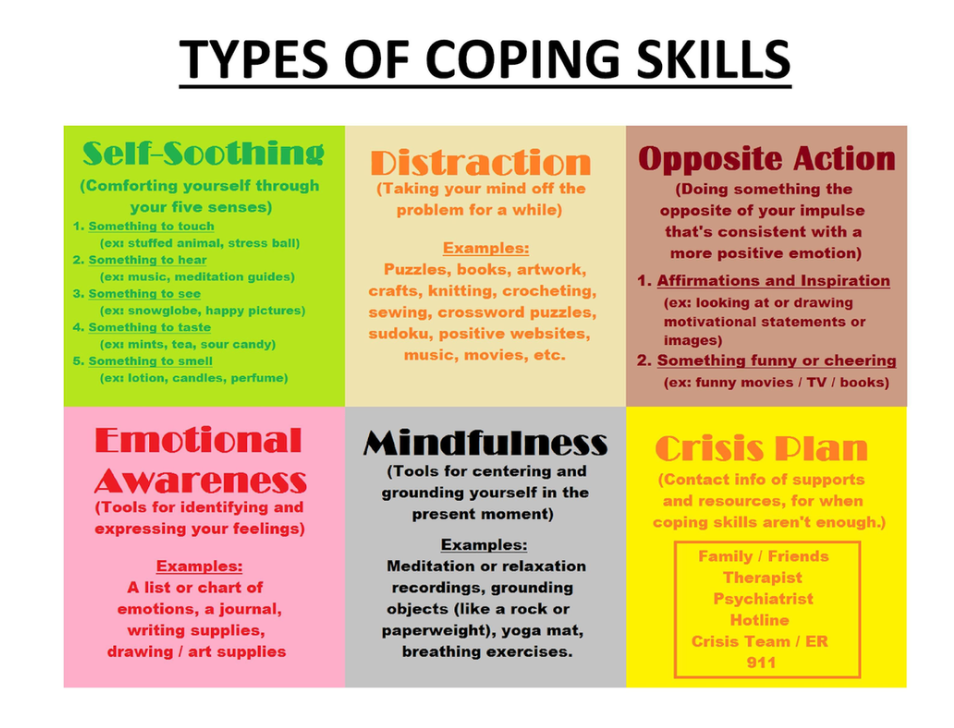
Coping skills:
Remember, those who self-harm are not looking for attention, rather, they may feel overwhelmed when dealing with difficult feelings and not have proper coping skills to regulate their emotions. Exploring healthy outlets to cope with the pain and slowly building upon each coping skill can delay or replace self-harm.
(Source: SAMHSA)

If you or someone you know needs support now, call or text 988.
September is also National Recovery Month
- A time to discuss the impact of recovery from substance use.
- According to the U.S. Department of Human Health and Services 2021 report, 1 in 3 adults had a substance use disorder.
- In the 2021 CDC report, there were 107,622 deaths from drug-related overdoses.
Let’s work to bring more awareness and light towards substance use disorder. Substance use is not a moral failing or lack of willpower, but a chronic disease. Recovery is possible with the proper treatment.
To read more about substance use disorder, click this link.
Let’s take a look at Action Steps, Protective Factors,
and Coping Skills

Protective factors:
- Contacts with providers (such as follow-up phone calls from a healthcare professional).
- Effective mental health care; easy access to a variety of clinical interventions.
- Feelings of strong connections to individuals, family, community, and social institutions.
- Strong sense of cultural identity.
- Problem-solving and conflict resolution skills.
- Healthy coping skills.

If you want to learn more about helping yourself, a loved one, or any individual experiencing a mental health challenge or crisis, you can join our Mental Health First Aid Training on Sept. 25 and 26. This course offers knowledge, insight, and tools to assist in a challenge or crisis. These tools can help save a life.
Thanks,

Allison LaRussa, B.A., CPS, RYT
Director, Health Humanities
The Wright Centers for Community Health and Graduate Medical Education