A 2015 white paper published by a physician staffing firm called it a “silent shortage.” In a country gripped by the grim phenomenon dubbed “deaths of despair,” “it” is a severe and under-appreciated shortage of the very people with the skills and knowledge necessary to reverse the trend. Our region, like the rest of the nation, needs psychiatrists.
How bad is the problem? The late Richard Cooper, M.D. of the University of Pennsylvania, a noted national authority on physician supply, distribution and utilization, finds that a population of 100,000 should have 14.7 psychiatrists, or one for every 6,800 people. The counties of northeastern Pennsylvania average about 8.5, according to Dartmouth Atlas of Health Care. Moreover, the few psychiatrists we have must cope with three of the “Top 10” diseases most associated with lost quality of life. According to the World Health Organization (WHO), “unipolar depressive disorders” are the No. 1 cause of medical disability in the United States. Dementias, including Alzheimer’s, and alcohol and ecstasy disorders come in at No. 3 and No. 4. The escalating opioid crisis is, no doubt, claiming its place as it climbs the rank order.
Despite the suffering and lost years of life caused by (often undiagnosed) behavioral and mental health diseases, we still cling to outdated ideas about psychiatry like, “If people just had more willpower and determination, they’d “snap out of” their depression,” and, “Addiction is a sign of moral weakness, so patients have only themselves to blame.” The healthcare system is fragmented; it is not built on resiliency, but on brokenness. The persistence of these discredited notions about mental health has led to what should be a national wake-up call – for the first time in decades, mortality rates for a certain U.S. demographic (whites aged 45 to 54 – an important demographic in NEPA) rose by half a percent a year since 1998. The cause of these deaths is overwhelmingly attributed to suicide and addiction. No other rich country has experienced anything like these “deaths of despair.” As Angus Deaton, an economist, Nobel Laureate and co-author of the paper which first identified the trend, told the Washington Post, “That means half a million people are dead who should not be dead. That’s about 40 times the Ebola stats. You’re getting up there with HIV-AIDS.”
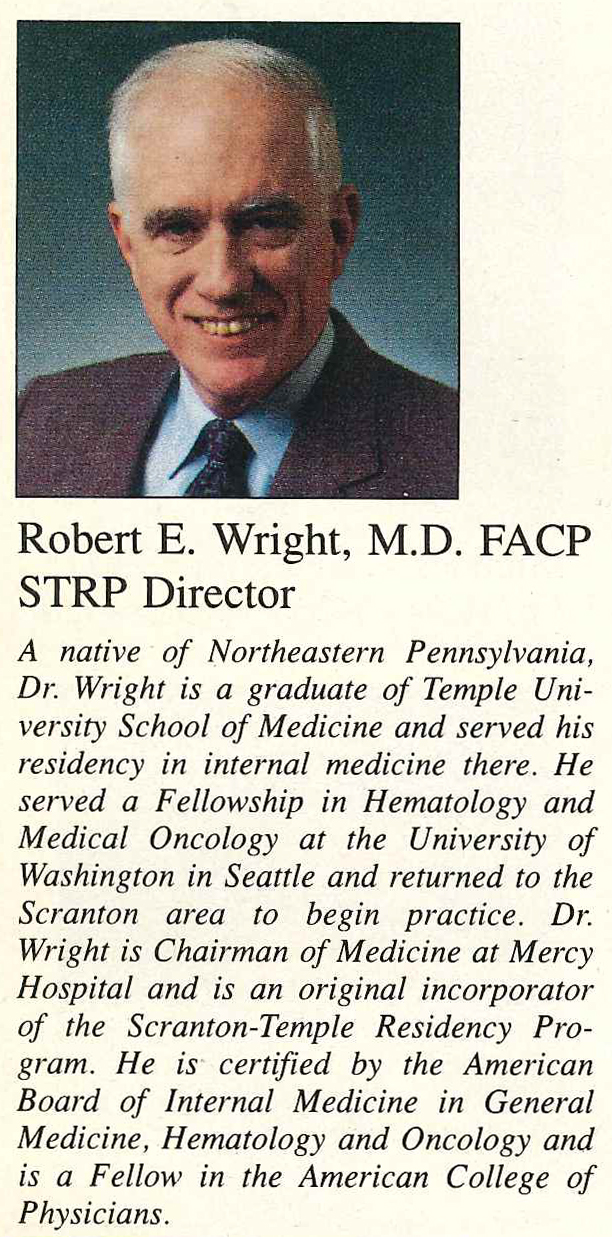
Although Dr. Deaton’s ground-breaking report was published in 2015, a Community Health Needs Assessment conducted by the Institute for Public Policy and Economic Development in 2012 identified mental and behavioral health challenges, including higher-than-national-average suicide rates, in our region. That’s when Geisinger Commonwealth School of Medicine convened an advisory group for the school’s Behavioral Health Initiative (BHI). The advisory committee was charged with identifying gaps in access to mental health services in several counties of northeastern Pennsylvania. Market intelligence firm, Open Minds, working on behalf of BHI, concluded that a seven-county region of NEPA would need to increase its number of psychiatrists by 40 percent simply to meet current need. With that data, at the time of its formal launch in 2015, BHI generated a key recommendation: the School of Medicine and The Wright Center should co-create a psychiatry residency program to train new doctors in this desperately needed specialty. All parties humbly recognized a new psychiatry residency could serve as an educational fulcrum for much larger inter-professional workforce development initiatives by leveraging this powerful, inclusive partnership.
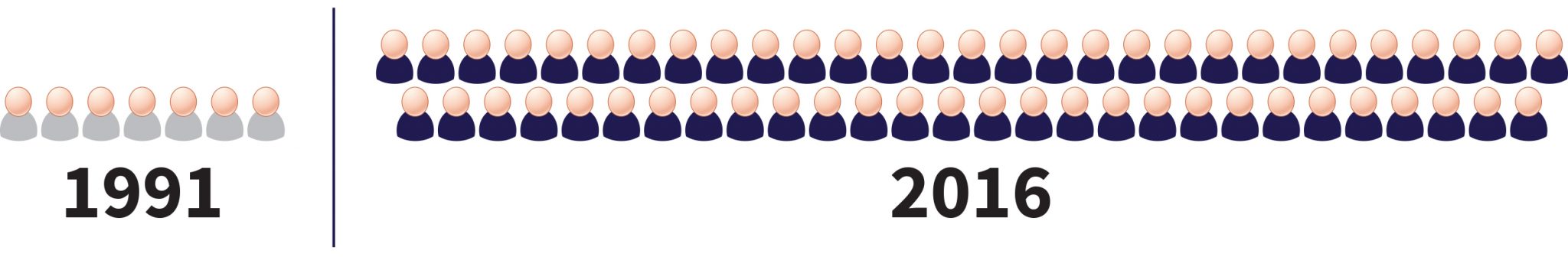
This July, just two years after BHI’s 2015 launch (light speed in academia), we are proud to announce that The Wright Center will welcome four residents to its brand-new, ACGME (Accreditation Council for Graduate Medical Education) accredited psychiatry residency program. The fact that one of these new psychiatry residents is also a 2017 graduate of Geisinger Commonwealth School of Medicine makes this accomplishment all the more meaningful. Psychiatry training takes four years, so once all four classes are filled, we will train 16 residents here in Scranton and Wilkes Barre, and graduate four newly-minted psychiatrists per year.
The School of Medicine and The Wright Center have long been partners committed to addressing the specific health needs of our community, with a formal commitment solidified through the signing of a Memorandum of Understanding in 2015. That’s why we and our BHI partners worked so swiftly and purposefully to establish the psychiatry residency program despite the significant challenges of funding and accreditation. Wide-scale community collaboration, including Scranton Counseling Center’s generosity with the time and the expertise of Sanjay Chandragiri, MD, our pioneering program director, has generated the opportunity for four new doctors to learn how to treat and heal patients struggling with behavioral health issues. In this way, our community is taking an important step toward reducing “deaths of despair” in our region, replacing years lost to disability with years of enhanced health and wellbeing.
Linda Thomas-Hemak, MD is President/CEO of The Wright Center Medical Group and The Wright Center for Graduate Medical Education, the largest HRSA-funded Teaching Health Center (THC) consortium in the United States
Terri Lacey, RN is executive director of Geisinger Commonwealth School of Medicine’s Behavioral Health Initiative, a collaborative, community-based initiative to address systemic gaps in mental health and substance abuse services available in northeastern and north central Pennsylvania.