Dr. Linda Thomas-Hemak, president and CEO of The Wright Centers for Community Health and Graduate Medical Education, received the 2024 Wilford Payne Health Center Mentor Award from the Pennsylvania Association of Community Health Centers (PACHC) in recognition of her outstanding leadership, mentorship, and dedication to nurturing future health care leaders.
She accepted the award, part of PACHC’s Awards for Primary Care Excellence (APEX), on Oct. 8 during the organization’s Annual Conference and Clinical Summit in Lancaster, Pennsylvania.
“I am truly humbled and honored to receive the Wilford Payne Health Center Mentor Award, an Award for Primary Care Excellence or APEX Award from the Pennsylvania Association of Community Health Centers,” said Dr. Linda Thomas-Hemak, president and CEO of The Wright Centers for Community Health and Graduate Medical Education. “Mentorship is a sacred privilege and crucial leadership responsibility at The Wright Center.
“This recognition reflects the collective work of my extraordinary colleagues and our shared commitment to cultivating and inspiring the next generation of compassionate, skilled, and visionary health care leaders. Inspired by the impact of Wilford Payne, whose leadership work advanced and elevated the health center movement in our state and nation, I remain deeply committed to empowering those who choose to devote their careers to public service and the health center movement. Mentorship force multiplies our personal impact on the health and well-being of our communities, carrying it forward to a preferred future.”
The award is given in memory of Wilford Payne, co-founder and former CEO of Primary Care Health Services in Pittsburgh, who devoted his life to expanding access to health care for underserved communities and mentoring the next generation of health center leaders. It recognizes individuals who see and nurture the potential in others, support their growth and development, and inspire through exemplary leadership.
Concurrent with her executive responsibilities, Dr. Thomas-Hemak is also quintuple board-certified in internal medicine, pediatrics, obesity medicine, addiction medicine, and nutrition. She sees generations of patients at The Wright Center for Community Health’s Mid Valley Practice in Jermyn.
She is a graduate of Scranton Preparatory School and the University of Scranton. After graduating as a Michael DeBakey Scholar from Baylor College of Medicine in Houston and completing Harvard’s Combined Internal Medicine/Pediatrics Residency Program in Boston, she returned to Northeast Pennsylvania, joining The Wright Center in 2001, becoming president in 2007, and CEO in 2012.
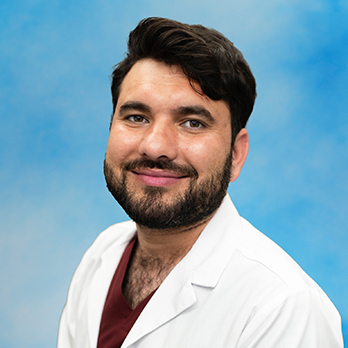
Dr. Linda Thomas-Hemak, M.D., FACP, FAAP
Dr. Thomas-Hemak has spearheaded The Wright Center for Community Health’s transformation into one of the first state-designated Opioid Use Disorder Centers of Excellence in 2016 to improve access to substance use disorder treatment. Amid surging obesity rates, she guided physicians at The Wright Center to become board-certified in obesity medicine.
As president/CEO, she has expanded the nonprofit safety net to 11 primary and preventative care health centers in Lackawanna, Luzerne, Wayne, and Wyoming counties and a mobile medical and dental unit called Driving Better Health. Each provides affordable, high-quality, nondiscriminatory, high-quality, responsive whole-person primary health services to individuals of all ages, regardless of their insurance status, ZIP code, or ability to pay.
Her leadership also transformed The Wright Center for Graduate Medical Education into one of the nation’s largest Teaching Health Center Graduate Medical Education Safety-Net Consortiums (GME-SNC) funded by the U.S. Health Resources and Services Administration. The GME-SNC effectively addresses the national shortage and uneven distribution of primary care physicians, as well as health and workforce shortages, by maximizing public investments in primary care, responsive community health services, and innovative physician and interprofessional workforce development, along with other vital and related public health initiatives.
Under Dr. Thomas-Hemak’s stewardship, The Wright Center has achieved numerous prestigious distinctions, including its designation as a Federally Qualified Health Center Look-Alike in 2019, which unlocked essential federal resources for the region and greatly expanded access to high-quality, comprehensive primary care for local families. It has also been recognized as a Top 30 Site for National Primary Care Innovations by the Robert Wood Johnson Foundation and, in 2024, was inducted into the esteemed American Medical Association’s ChangeMedEd Consortium.
A founding board member of the Geisinger Commonwealth School of Medicine, Dr. Thomas-Hemak is governor of the eastern region of the American College of Physicians’ Pennsylvania Chapter, the nation’s largest medical-specialty organization. She is a member of the Council on Graduate Medical Education for the U.S. Health Resources and Services Administration; vice president and founding board member of the American Association of Teaching Health Centers; governing board chair and executive committee member of the Northeast Pennsylvania Area Health Education Center; and advisory board member of the Health Federation of Philadelphia’s Health Center Controlled Network. She also serves as a board member for the Keystone Accountable Care Organization, The Institute, and the Center for Health and Human Services Research and Action.
In recognition of her advocacy and leadership, Dr. Thomas-Hemak has received numerous awards, including the Ann Preston Women in Medicine Award, the Hometown Scholar Advocate of the Year Award, the National Association of Community Health Centers Elizabeth K. Cooke Advocacy MVP Award, and City and State Pennsylvania’s 2024 Trailblazers in Healthcare.
She and her husband, Mark, reside in Jermyn and have three children, Mason, Maya, and Antoinette. Dr. Thomas-Hemak is the daughter of the late William Thomas and Johanna Cavalieri Thomas, who lives in Archbald.